“One of these individuals is a seven-year-old boy in remission from Leukemia who is now unable to access follow-up—and potentially lifesaving—treatments,” said local advocacy groups.
Hundreds of thousands of poor Floridians have been kicked off Medicaid in recent weeks as their Republican governor, Ron DeSantis, travels the country for his 2024 presidential bid and rakes in campaign cash from big donors.
Florida is one of more than a dozen states that have begun unwinding pandemic-era rules barring states from removing people from Medicaid during the public health emergency. Late last year, Congress reached a bipartisan deal to end the so-called continuous coverage requirements, opening the door to a massive purge of the lifesaving healthcare program.
A dozen states have released early data on the number of people removed from Medicaid as they restart eligibility checks, a cumbersome process that many people ultimately fail to navigate.
So far, the numbers are alarming: More than 600,000 people across the U.S. have been stripped of Medicaid coverage since April, according to a KFF Health Newsanalysis of the available data, and “the vast majority were removed from state rolls for not completing paperwork” rather than confirmed ineligibility.
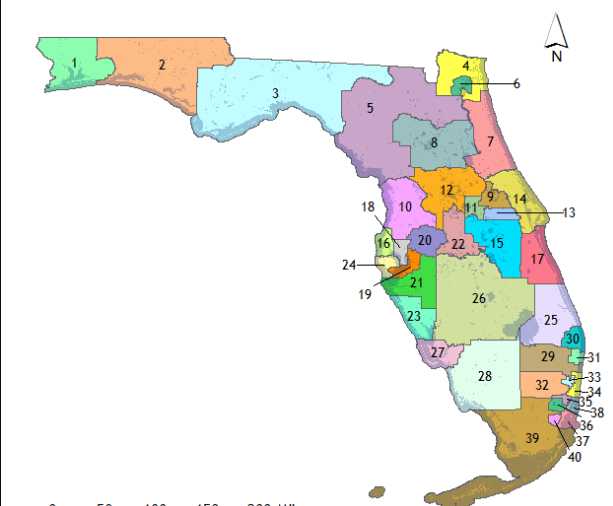
Nearly 250,000 people who have been booted from Medicaid live in Florida, whose governor is a longtime opponent of public healthcare programs. As HuffPost‘s Jonathan Cohn wrote Sunday, DeSantis “has refused to support the ACA’s Medicaid expansion for the state, which is the biggest reason that more than 12% of Floridians don’t have health insurance.”
“That’s the fourth-highest rate in the country,” Cohn noted.
But DeSantis, who has said he wants to “make America Florida,” appears unmoved by the staggering number of people losing Medicaid in his state as he hits the campaign trail. The governor relied heavily on large contributors to bring in more than $8 million during the first 24 hours of his presidential bid.
Prior to formally launching his 2024 campaign, DeSantis traveled the country in private jets on the dime of rich and sometimes secret donors, and he is currently facing a Federal Election Commission complaint for unlawfully transferring more than $80 million from a state committee to a super PAC supporting his White House bid.
“Families with children have been erroneously terminated, and parents are having trouble reaching the DCF call center for help with this process.”
Late last month, DeSantis’ administration insisted it “has a robust outreach campaign” aimed at ensuring people are aware of the hoops they have to jump through to keep their Medicaid coverage, such as income verification.
In Florida, a four-person household must make less than $39,900 in annual income to qualify for Medicaid.
The state’s early data indicates that 44% of those who have lost coverage in weeks were removed for procedural reasons like failing to return paperwork on time.
The figures have drawn alarm from local advocates, who urged DeSantis late last month to pause the Medicaid redetermination process after hearing reports of people losing coverage without receiving any notice from Florida’s chronically understaffed Department of Children and Families (DCF).
“One of these individuals is a seven-year-old boy in remission from Leukemia who is now unable to access follow-up—and potentially lifesaving—treatments,” a coalition of groups including the Florida Policy Institute and the Florida Health Justice Project wrote to DeSantis. “Families with children have been erroneously terminated, and parents are having trouble reaching the DCF call center for help with this process. Additionally, unclear notices and lack of information on how to appeal contribute to more confusion.”
Citing Miriam Harmatz, advocacy director and founder of the Florida Health Justice Project, KFF Health Newsreported last week that “some cancellation notices in Florida are vague and could violate due process rules.”
“Letters that she’s seen say ‘your Medicaid for this period is ending’ rather than providing a specific reason for disenrollment, like having too high an income or incomplete paperwork,” the outlet noted. “If a person requests a hearing before their cancellation takes effect, they can stay covered during the appeals process. Even after being disenrolled, many still have a 90-day window to restore coverage.”
The Congressional Budget Office recently estimated that, nationwide, around 15.5 million people are likely to lose Medicaid coverage over the next year and a half—including 5 million children—as states resume eligibility checks made necessary by a system that doesn’t guarantee healthcare to all as a right.
“Many people don’t realize that they’ve been disenrolled from Medicaid until they show up at the pharmacy to get their prescription refilled or they have a doctor’s appointment scheduled,” Jennifer Tolbert, director of state health reform at the Kaiser Family Foundation, toldThe Washington Post last week.
Common Dream’s work is licensed under a Creative Commons Attribution-Share Alike 3.0 License. Feel free to republish and share widely.
[content id=”79272″]