Chronic use of some drugs for heartburn and gastroesophageal reflux (GERD) speeds up the aging of blood vessels, according to a published paper in Circulation Research (early online), an American Heart Association journal. This accelerated aging in humans could lead to increased cardiovascular disease, vascular dementia and renal failure.
These findings by a Houston Methodist Research Institute team are a progression of the work that John Cooke, M.D., Ph.D., began more than five years ago, and support recent epidemiological and retrospective studies that observed associations between the long-term use of proton pump inhibitors (PPIs) and an increased risk of heart attack, renal failure and dementia.
PPIs like esomeprazole (Nexium) are widely used for the treatment of GERD. These medications are sold over-the-counter in the United States so medical supervision is not required. While these drugs are effective when taken as prescribed, they were not approved for long-term use and evidence suggests that up to 70 percent of PPI use may be inappropriate.
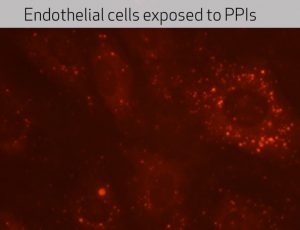
Cooke, the paper’s senior author, and team showed that chronic exposure to PPIs accelerated biological aging in human endothelial cells which line the inside of blood vessels. When healthy, human endothelial cells create a Teflon-like coating that prevents blood from sticking. When older and diseased, the endothelium becomes more like Velcro, with blood elements sticking to the vessel to form blockages.[xyz-ihs snippet=”adsense-body-ad”]
“When we exposed human endothelial cells over a period of time to these PPIs, we observed accelerated aging of the cells,” Cooke said. “The PPIs also reduce acidity in lysosomes of the endothelial cell. The lysosomes are like cellular garbage disposals and need acid to work properly. We observed cellular garbage accumulating in the endothelial cells, which sped up the aging process.”
Cooke suspects that this may be the unifying mechanism that explains the increased risk of heart attack, renal failure and dementia observed in long-term PPI users.
“These drugs do not seem to adversely affect the heart and blood vessels when taken for a few weeks. However, we urgently need studies to assess the impact of long-term use of these drugs on vascular health in a broad patient population. We also need to consider if these drugs should be so accessible without medical supervision.”
Cooke’s earlier work identified at a molecular level that PPIs might cause long-term cardiovascular disease and increase a patient’s heart attack risk. That work led to a collaborative study with Stanford University colleagues (PLOS ONE, June 2015) to show that in two large populations of patients, adults who used PPIs were between 16 to 21 percent more likely to experience a heart attack than people who didn’t use the commonly prescribed antacid drugs.
Cooke, who holds the Joseph C. “Rusty” Walter and Carole Walter Looke Presidential Distinguished Chair in Cardiovascular Disease Research, said while PPIs were shown to affect vascular aging, H2 blockers like ranitidine did not adversely affect the endothelium. Brand examples of H2 blockers are Zantac and Tagamet.
The FDA estimates about 1 in 14 Americans have used a PPI. In 2009, PPIs were the third-most taken type of drug in the U.S., and are believed to account for $13 billion in annual global sales. In addition to GERD and heartburn, PPIs treat a wide range of disorders, including infection by the ulcer-causing bacterium Helicobacter pylori, Zollinger-Ellison syndrome, and Barrett’s esophagus. PPIs come in a variety of forms, always ending with the suffix “-prazole,” and other brand examples include Prilosec and PrevAcid.
Additional researchers who collaborated with Cooke on the Circulation Research paper were: Gautham Yepuri, Roman Sukhovershin, Timo Z. Nazari-Shafti (Houston Methodist Research Institute, Houston, TX); Yohannes T. Ghebre (Baylor College of Medicine); and Michael Petrascheck (The Scripps Research Institute, La Jolla, CA).
Houston Methodist: Links Between PPIs and Vascular Aging from Houston Methodist on Vimeo.
This research was supported by grants from National Institutes of Health (U01HL100397 and K01HL118683) and the Swiss National Science Foundation (P2FRP3_151676).
Source: Houston Methodist [xyz-ihs snippet=”Adversal-468×60″]



