In early 2020, at the beginning of the pandemic, we knew almost nothing about COVID-19. How did it spread? Who would get sick? How could we protect ourselves and each other?
In early 2020, at the beginning of the pandemic, we knew almost nothing about COVID-19. How did it spread? Who would get sick? How could we protect ourselves and each other?
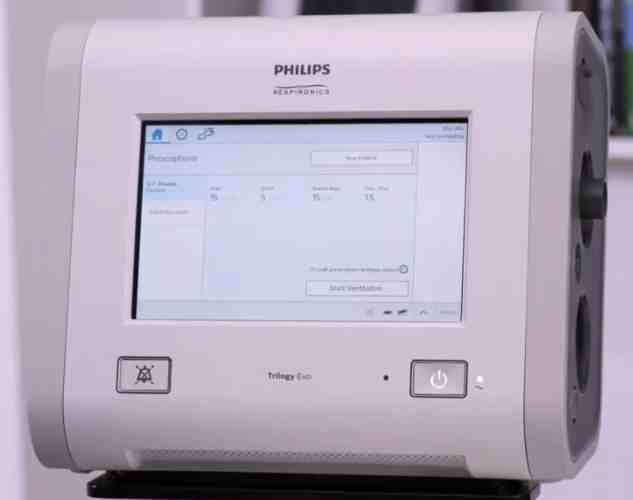
We saw hospitals being built and overflowing, first in China, then Italy and New York. Morgues filled across the world as health care facilities made desperate pleas for ventilators, personal protective equipment and additional health care workers. Here in Alaska, we scrambled to make our own testing supplies and to quickly build up our health care capacity. Public health worked to fill the gaps and supported the health care system by educating providers and the public, supporting health care staffing needs, and setting up testing, treatment and vaccination centers. Alaska’s health care providers worked tirelessly to protect our communities, and I will be forever grateful for the dedication and resilience of our health care workforce.
Today, we have wonderful tools available to fight COVID-19, including safe and effective vaccines for everyone six months or older, giving nearly all of us the opportunity to train our immune systems to defend against the worst of a COVID infection. And for Alaskans with compromised immune systems who may not mount an adequate immune response from vaccination, we have Evusheld: a preventive monoclonal antibody therapy that protects people before they are exposed to COVID.
While prevention is always best, we also now have multiple COVID-19 treatment options – including antiviral pills – widely available at clinics, doctors’ offices, and pharmacies in nearly every community in Alaska. The vast majority of Alaskans meet the broad qualifications for these treatments, which are highly effective at reducing the risk of hospitalization and death for people who get COVID-19. These treatments work regardless of whether a person is vaccinated, but they require a prescription and work best if they are taken very soon after symptoms first arise or a patient receives a positive COVID test. Family doctors, nurse practitioners, pharmacists, and others must be knowledgeable about the available treatment options, and people need to have timely access to testing and a health care provider. [content id=”79272″]
Some treatment options may be going away altogether in the months ahead. Monoclonal antibodies were among the first outpatient treatment options available, and Alaska stood up the first state-run infusion center in the country. Monoclonals have been an invaluable tool. Clinics around the state rose to the challenge to deliver the medications to Alaskans, often free of charge and without an appointment. But as useful as monoclonals have been, they were never meant to be a long-term solution. For one, they’re difficult to administer: they require injections or infusions at specialized clinics. They’re also costly to produce, making them one of the most expensive drug classes out there. We have also seen rapid changes in the effectiveness of monoclonal antibodies as the virus has evolved, rendering all of our original monoclonals ineffective, unlike COVID antiviral medications, which continue to work well against newer variants.
Another issue is that states are reliant on the federal government for our monoclonal antibody supply. Alaska’s supply of bebtelovimab, the only monoclonal antibody that remains effective against Omicron, is becoming depleted. We learned this week that the federal government will be supplying more bebtelovimab to states, but we do not anticipate the supply will last us much past August. The State of Alaska will continue to distribute all therapeutics we receive from the federal government.
For these reasons, clinicians and patients should not depend on monoclonal antibodies to be around for the treatment of COVID-19. Monoclonal antibodies have served us well, but they are less useful now compared to effective antiviral medications like Paxlovid and molnupiravir. There are several advantages to these new antiviral medications: first, these drugs can be taken orally as pills, making it much more convenient for patients. Second, they are also much less expensive to produce and easier to distribute to the farthest corners of our state. And third, they are effective against all current COVID variants.
Oral antivirals are abundant in supply, as is the antiviral remdesivir which is administered by infusion. But supply is just one part of the solution. Patients can’t use these lifesaving drugs without a prescription. That means people need to get tested as soon as they suspect they have COVID, then should talk quickly with a health care provider about whether COVID medications are right for them. Providers need to be ready to help their patients by assessing their risk factors and writing prescriptions when needed.
It is imperative that my fellow Alaskan health care professionals learn about all of the available COVID treatment options and ensure that their patients are staying up to date on vaccinations. Currently we are seeing yet another increase in hospitalizations for those over 50 in Alaska, but we have the tools to prevent this.
In the months ahead, the burden of prescribing, dispensing and ultimately paying for COVID-19 treatments is shifting from public health into the health care sector. Public health will continue to stand in the gaps where we can, working to reduce the burden of COVID and other diseases as promote and protect the health and well-being of every Alaskan.
This pandemic has been long, hard, and at times confusing. We continue to share information at covidrx.alaska.gov, where you will find updates and resources for the public, as well as tools for clinicians to help decide which medication is right for your patient, and medication order forms. For any questions, you can call the Alaska COVID Helpline at 907-646-3322. Hours are 9 a.m. – 6:30 p.m. on weekdays.
COVID-19 was the third-leading cause of death in Alaska in 2021. Because the worst effects of the disease are now preventable and treatable, we expect the threat of COVID to decrease over time. However, that expectation comes with a caveat: vaccination, early treatment and infection control practices can save lives, prevent hospitalizations, and reduce long-COVID, but only with professional diligence and personal effort.
It will continue to take all of us to make choices that protect our health, and to care for ourselves, our patients, our family and friends and our community. We also must continue to come together to make our systems of care work towards improving the health of every Alaskan.
Dr. Anne Zink, M.D., is a board-certified emergency physician and Alaska’s chief medical officer.[content id=”79272″]