Newswise — In the war against obesity, one’s own fat cells may seem an unlikely ally, but new research from the University of California, San Francisco (UCSF) suggests ordinary fat cells can be reengineered to burn calories.
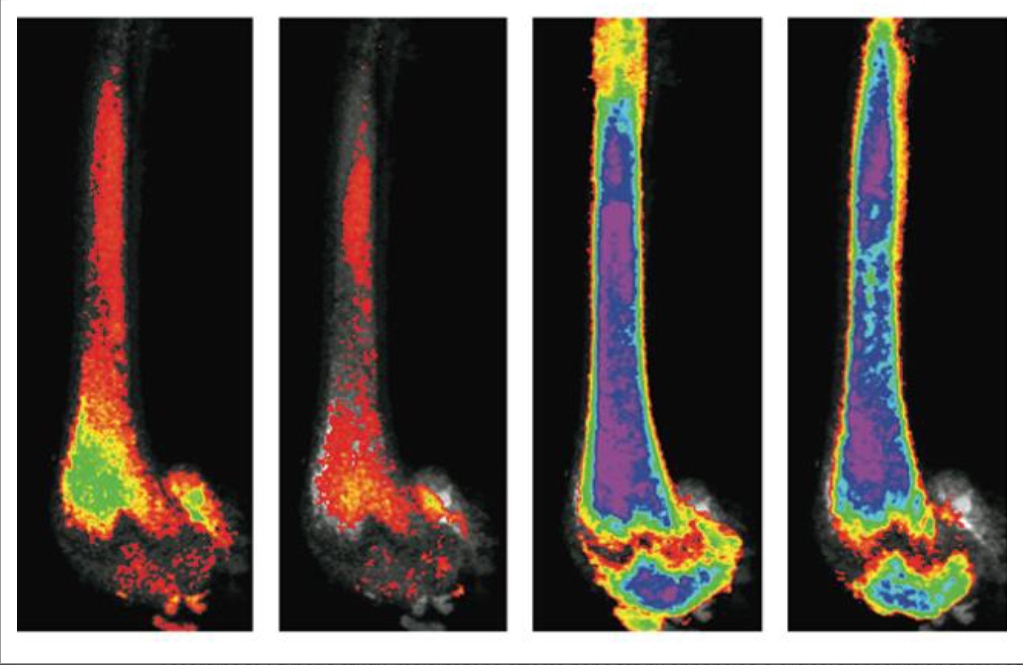
While investigating how a common drug given to people with diabetes works in mice, a UCSF team discovered that a protein called PRDM16, found in both men and mice, can throw a switch on fat cells, converting them from ordinary calorie-storing white fat cells into calorie-burning brown fat cells.
This discovery makes PRDM16 a possible target for future obesity drugs. Compounds that promote the action of this protein may help people burn calories faster. Though they would have to prove safe and effective in the clinic, such compounds would represent a completely different approach to weight loss. Existing diet drugs aim to restrict the intake of calories — by blocking the absorption of fat in the gut, for instance, or by decreasing appetite.
“If you think about the energy balance, the other way to tackle obesity is through energy expenditure,” said Shingo Kajimura, PhD, who led the research in the UCSF Diabetes Center and the Department of Cell & Tissue Biology in the UCSF School of Dentistry. The work is published this week in the journal Cell Metabolism.
Where Brown Fat Comes From
Scientists believe that brown fat originally evolved in early mammals as a defense against the cold. It helps them maintain their body temperature and thrive in the face of challenging environmental extremes. Not all animals share this ability.
Many animals, like lizards, are “cold blooded” or exothermic. They maintain their body temperature through completely external means, sunbathing at certain times of the day and huddling in warm, protective places at night. This naturally limits their range and explains why lizards, so abundant in tropical climates, are far rarer in cold climates.
“Warm-blooded” mammals, on the other hand, are endothermic. They produce heat internally by a variety of means: shivering, sweating and regulating the size of their blood vessels. Brown fat also contributes by burning fatty acids, which heats the blood coursing nearby, and in turn warms the body.
Though scientists once thought new brown fat was only made in babies, we now know that the human body is capable of creating new brown fat cells throughout life. And in recent years, doctors also have discovered the amount of brown fat in the body is inversely proportional to the likelihood of obesity — the more brown fat people have, the less chance they are obese.
The possibility of exploiting brown fat for weight loss became tantalizing after clinical evidence showed that certain drugs could alter the amount of brown fat a person has. In particular, a common class of drugs given to people with diabetes called PPAR-gamma ligands has been shown to increase brown fat. But scientists never understood why.
Now Kajimura and his UCSF colleagues have demonstrated how it works. In their research, they showed that PPAR-gamma interacts with the protein PRDM16, making it more stable and leading to its accumulation inside cells. This essentially throws a genetic switch and converts the white fat cells to brown — at least in mice.
The question remains whether it is possible to do this in people as well, and if so, how. While new drugs that target this protein may be years away, knowing the target may speed their development, Kajimura said.
The question is no longer how do we make brown fat, he added. Instead it now becomes a more specific question: “Can we simply stabilize this protein?”
The article, “PPAR-gamma agonists induce a white-to-brown fat conversion through stabilization of PRDM16 protein” by Haruya Ohno, Kosaku Shinoda, Bruce M. Spiegelman, and Shingo Kajimura appears in the March 7 issue of the journal Cell Metabolism. See: https://dx.doi.org/10.1016/j.cmet.2012.01.019
This work was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, one of the National Institutes of Health.
UCSF is a leading university dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care.