An extensive review of scientific literature indicates that depression should be added to the list of risk factors associated with heart disease. Others include obesity, diabetes, high blood pressure and smoking.
A 12-person panel of experts that included Robert M. Carney, PhD, and Kenneth E. Freedland, PhD, both professors of psychiatry at Washington University School of Medicine in St. Louis, made the recommendation to the American Heart Association (AHA).
Their findings are published online as a scientific statement in the journal Circulation.
The group sifted through hundreds of studies looking at the link between depression and heart problems. Most of the studies found that depression made people more likely to have a heart attack or die from heart disease.
“The findings didn’t surprise us,” said Carney. “Many studies have reported that depression predicts increased mortality, but it’s rare to delve into this kind of research as deeply and as carefully as we have. Although we suspected we would find this link, having gone through all of these studies and conducted such a careful evaluation, we are more confident than ever that depression is a risk factor for mortality in people who have heart disease.”
Carney and Freedland were chosen to be part of the expert panel because they have been studying depression’s effects on heart disease for more than 25 years, first reporting in 1988 that depression predicts an increased risk of cardiac problems in patients with existing heart disease. Hundreds of studies have been conducted since then, and most have supported their initial observation.
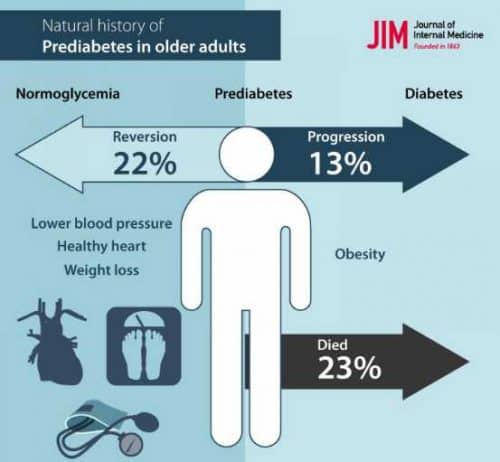
Carney noted that when people lose weight, lower their blood pressure or quit smoking, their risk of heart disease is lowered. But so far, no studies have shown that treating depression lowers cardiac risk.
“Unfortunately, very few studies have looked at that question,” Carney explained. “And only one study has included enough subjects to determine whether treating depression could lower the risk of having a heart attack or dying from heart disease. Treatment did not lower the risk of heart attack or death, but that was the first study of its kind. More clinical trials are needed to identify treatments that may improve heart health along with depression.”
Part of the problem is that the available treatments don’t work for everyone. Even the best therapies for depression lead to remission in only about one of every two depressed patients.
But Carney and Freedland are set to begin a new clinical trial to evaluate whether a different approach to treatment can be more successful in alleviating depression and lowering the risk of future cardiac events.
“We believe better depression treatments may improve survival,” Carney said. “More effective treatments certainly will improve a patient’s quality of life. More research will be needed, though, before we can say treating depression can improve heart health or survival in patients with heart disease.”
What is known with certainty at this point, he said, is that not treating depression can have negative effects on health and quality of life.